




Saturday June 9, 2018
Morgan Livingstone CCLS discusses how the external environment influences infant mental health, and the varied ways parents and medical professionals can help babies cope and thrive through medical interventions.
“An infant’s cry cries out to be heard”. – Anonymous
I love infants. Anyone’s baby will do, but my passion for working with infants has been a part of who I am since I was a child. There is something magical about a baby. A new life. A new person filled with possibility and promise.
In the first few months of life, just as parents are busy learning to read their baby’s cues, the baby also learns to read a parent’s emotional and social cues – the reciprocal back-and-forth experience. Infants sense and respond to their parent’s moods and emotions.
Although an infant’s language lacks words, it is rich with facial expressions, crying, cooing, gurgling or withdrawal. Young infants experience a wide range of human emotions, including sadness and fear. We are just beginning to understand the depths of feelings, emotions and stress responses infants can experience.
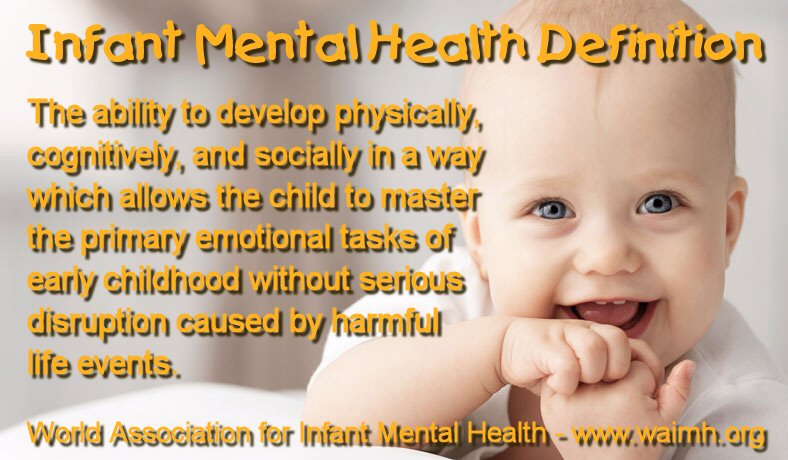
Infant mental health is gaining greater awareness and attention. The scientific, medical and mainstream discourse includes so much more about how nature (our biology), and nurture (our environment), form early experiences that shape the brain, affecting lifelong health, behaviour and learning. No other stage depends more on the external environment for growth and development. Very young children, whose brains are still extremely malleable to environmental stress, also respond differently to external stress than older children.
Infants are amazingly resilient. With the right love, attention and support, they can even learn to survive and thrive through early childhood cancer. A family’s retinoblastoma journey can begin in many different ways, but for most families, it all centers around an infant. Their baby.
The reciprocal relationship between infants, parents and the greater world is important to consider when facing a serious illness with many possible directions for treatment. No path is best when determining the way forward for an infant diagnosed with retinoblastoma; each journey has multiple considerations, both medically and personally. The essential core focus must always be the best possible outcomes for the life of the infant. From here, parents and the medical team can include vital strategies to best support the infant’s coping and mental health needs as they begin their medical experience.
Here are seven helpful areas caregivers can focus on to support an infant’s mental health during their retinoblastoma experience.

A baby benefits from supportive massage during medical care.
Pain in infants should be prevented and relieved as much as possible because pain can impact recovery, and cause significant distress, anxiety and fear. This often increases resistance to future procedures, and can affect the infant’s normal development. The limited emotional and social skills of young infants and children hinders their ability to cope with pain, so if their pain is under-treated, they potentially suffer even more.
Pain experienced at this early age may also have a long–lasting effect on future response to pain. Pain can affect an infant’s ability and desire to eat, the quality of their sleep, energy levels, mood, and their relationships with others.
During retinoblastoma surveillance and treatment, infants may experience routine painful procedures that will affect them both physically and mentally. Knowing this empowers parents to finding the right pain management approach early on.
The decision of therapy or medication appropriate for an infant’s pain should be taken jointly by the parents and the medical team. Since infants don’t always express discomfort easily or clearly, parents can help doctors assess pain by looking at cues and reporting their baby’s behaviors that all infants use to communicate.
Non-pharmacological pain management strategies are helpful and easy to provide. Sucking can help infants cope, so offer breast or bottle feeding (when possible), or a soother/pacifier to promote non-nutritive sucking. At most clinics and hospitals, sucrose (sugar water) can be given to an infant immediately before a painful procedure – the introduction of a sweet liquid promotes vigorous sucking. Many hospitals and clinics use pharmaceutical sucrose, so request it where possible. If it is not available, you can advocate for it.
The following video demonstrates supporting newborn babies through painful procedures using breastfeeding, bottle feeding, positions for comfort, sucrose and pacifiers.
This is the next video in the series, about supporting babies over 2 months.
Non-verbal signals pass between people of all ages all the time. Infants communicate without words by the way they move their body, the funny noises they make, and their different facial expressions. By watching your baby’s subtle and not so subtle cues, cues, you can often learn how they are feeling and when they need or want something.
You can create your own cues for certain daily routines. For example, using specific actions or words to signal a transition into diaper changes, mealtimes, nap times, travel time and playtimes. By using a particular song or word, you are preparing your baby for the transition. Listening, looking and feeling for your infant’s response helps you learn from them, and your baby also learns from you.

A father supports his baby with a chest to chest comfort position.
Comfort positions are a vital part of changing the medical experience and giving children, even infants, choices that include comfort from a parent. The wide variety of positions all have one common goal – helping kids feel better supported by parents while completing necessary medical procedures.
By exploring the different comfort positions with your infant, you will find preferred positions for each routine procedure you can expect at appointments. You can even become an expert problem solver, figuring out creative positions for new or unexpected procedures. Check out WE C Hope’s helpful guide to comfort positions and this useful poster from Children’s Mercy Hospital.
It’s a fact: parents are a baby’s #1 coping tool during procedures, assessments and check-ups. Finding ways to support your infant through the seemingly endless appointments and painful procedures can feel challenging and overwhelming, but your presence can dramatically benefit your baby’s coping, recovery and overall wellbeing. Advocate to be present for all procedures, including anesthesia induction (referred to as “Parent’s Presence for Induction” – PPI).
You may be uncomfortable or unable to physically assist the medical team with your baby during a specific procedure. However, just remaining in the room during the procedure, verbally coaching your baby with calm and loving statements, can significantly boost their ability to cope. Your silent presence can provide support, even if you are too emotional to talk or sing. Your smell alone reassuring your baby that you are close by.
Here is a wonderful webinar discussing parental presence during induction of anesthesia.
Positive touch has the power to provide comfort, manage pain, increase bonding, foster healthy attachment and promote coping. Infant massage, containment holds (with hands or swaddling), resting hands, and loving hugs and snuggles can have a huge impact on your baby, and you too!
When babies have experienced necessary life- and sight-saving painful procedures during their retinoblastoma care, positive touch also helps them build a trusting relationship with their parents. Most importantly, positive touch communicates love – the giving and receiving of love.
Touch your baby often. Hugs, snuggles and massage are free, so give and receive daily!
See the images below for some effective containment holds and resting hand positions to support babies through medical procedures. Click on the image for a larger view.
In this infant swaddle, the baby is wrapped in a blanket, but the feet are left out of the blanket so the medical team can access them for a blood draw/heel stick. The infant will be well supported in the blanket and parents arms.
In this newborn containment hold, a parent gently but firmly holds the folded arms/hands of the infant across the infant’s chest to allow for regulation, and access to the infant’s eyes by the doctor or nurse.
These are resting hands/containment holds for an infant’s feet. Since many painful blood draws from the feet can cause infants to have sensitive feet, this hold helps them experience positive touch on their feet, and can be used at any time for fun. This can also be used when an infant is having an examination and the parent wants to support the infant, but is unable to hold the baby in their arms. In the newborn containment hold, a parent gently but firmly holds the infant’s legs from the thighs down to the feet.
6 month+ containment hold.
This containment hold is great for supporting a newborn infant or a bigger baby, 6 months and up. The baby rests on one side, arms and legs together in front of him. For the newborn hold, the parent places one cupped hand firmly on the infant’s upper back, neck and head, fingers resting behind the head and thumb resting over the baby’s shoulder and upper arm. The other hand rests on the small of the infant’s back, buttocks and legs. For the older baby, the parent places one cupped hand firmly on the back of the baby’s head, and the other hand on the small of the infant’s back, buttocks and upper thigh area.
We live in an overstimulating world, and the experience of medical interventions is especially so for a young child. Stimulating all the senses in a way that promotes healthy engagement and fosters development can be difficult, but it is possible. Dana Suskind MD, author of “30 Million Words: Building a Child’s Brain” (2015), suggests focusing on a few simple tasks you can practice in your daily life with an infant.
Like all humans, babies use their senses to process information, make decisions, connect with the world and relate to others. Sensory stimulation in infancy aids brain development and helps babies learn about and make sense of their world. There are many simple strategies you can use to explore all five senses with your baby and promote healthy stimulation. Discover more and try these practical suggestions for each of the senses.
Advocating for your baby’s unique, individual needs means finding effective ways to communicate with the medical team. This is so important, since small breakdowns in communication can cause many cascading challenges over the course of a baby’s medical experience. Good medical teams will encourage you to ask any questions you might have about appointments, procedures and treatments. Unless you tell them, they won’t know what you and your baby need and want so you can be and feel successful.
For example, tell them about the strategies you and your baby prefer for different appointments and procedures. Model your preferred positions of comfort to show the medical team how they benefit baby while still allowing the team to complete the necessary procedures and assessments.
Advocating all the time can seem exhausting. Doctors are experts in the management of retinoblastoma, but you are the expert in your baby. Working together as a collaborative team, parents and medical professionals open up opportunities for better care and improved outcomes. Communication is key. Ask questions, seek support, and problem solve together. Your baby will thank you.
Promoting infant mental health is both a serious task and an opportunity. Infants ‘speak’ about their social and emotional status in their own special language that parents, families and caregivers are increasingly coming to understand.
We all need to work together towards optimal health outcomes. Fostering resiliency and reducing the potential negative impact of early childhood illness must be a priority for all in the infant’s care team. In doing so, we respect the undeniable rights of the child in their healthcare experience.

A baby girl plays with an anesthetic mask after child life supported medical play at One Rb World 2017.

Morgan Livingstone is a Certified Child Life Specialist and Certified Infant Massage Instructor/Trainer. She is passionate about improved child life and psychosocial supports for children and families affected by retinoblastoma.
As the Child Life Officer of World Eye Cancer Hope, Morgan contributes to the website’s Child Life sections, and speaks globally about child life supports for children with retinoblastoma. Morgan provided enriched multi-day child life programming for children of all ages at both One Rb World in Washington, D.C. in October 2017 and the Canadian Retinoblastoma Research Advisory Board meeting in December 2017.
Morgan also writes and creates resources for children and adults, and participates in child life research studies. She won the inaugural Innovation Grant at Operation Smile for developing an APP that uses Virtual Reality to prepare children receiving cleft lip and palate surgery for their operation.
Download Morgan’s helpful parent manual for supporting children’s worries using Worry Eaters.